Peripheral neuropathy is a condition that affects the peripheral nerves, which transmit signals between the brain and the rest of the body. This can lead to a range of symptoms, including pain, numbness, tingling, and weakness, particularly in the hands and feet. For those living with peripheral neuropathy, physical therapy can be a crucial part of managing symptoms and improving overall quality of life.
Causes of Peripheral Neuropathy
Peripheral neuropathy has many possible causes, including:
– Diabetes
– Chemotherapy treatment
– Vitamin deficiencies
– Injuries or trauma
– Autoimmune disorders
Identifying and treating the underlying cause is an important first step in managing neuropathy symptoms.
How Physical Therapy Can Help
Physical therapists can create a customized treatment plan to address the specific symptoms of peripheral neuropathy, which may include:
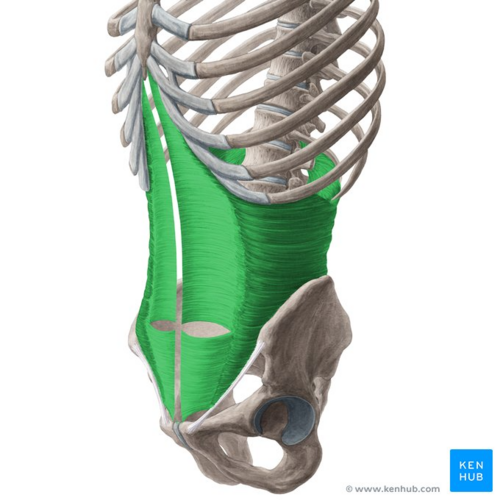
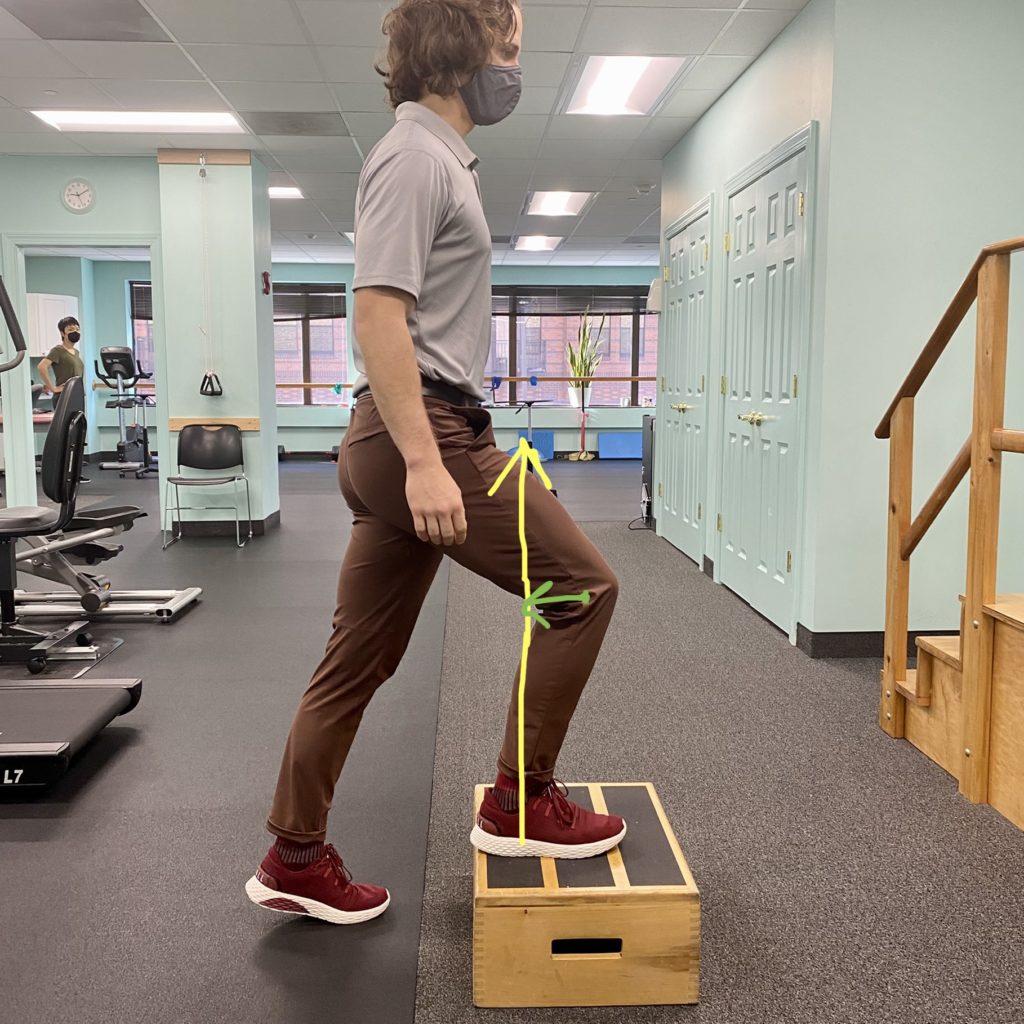
– Exercises to improve strength, balance, and flexibility
– Techniques to reduce pain and numbness, such as manual therapy and electrical stimulation
– Education on ways to protect the feet and hands to prevent further nerve damage
– Recommendations for assistive devices like braces or custom orthotics
By working closely with their physical therapist, patients can learn to manage their symptoms and maintain their independence.
Tips for Living with Peripheral Neuropathy
In addition to physical therapy, there are steps patients can take at home to help minimize the impact of peripheral neuropathy:
– Inspect feet and hands daily for any cuts, sores, or injuries
– Wear properly fitted, protective footwear
– Quit smoking and maintain healthy blood sugar levels if diabetic
Apply gentle heat or cold to reduce pain and swelling
With the right treatment approach and self-care strategies, many people with peripheral neuropathy are able to manage their symptoms and continue doing the activities they enjoy.